Categories
- Bariatric Surgery (11)
- Black Fungus (5)
- Bone Marrow transplant (3)
- Brain Tumor Surgery Navigation Technology (20)
- Cardiac Surgery (66)
- Cardiology (97)
- Computer navigation technology for joint replacements (20)
- Covid Vaccination (17)
- Critical Care (2)
- Dental (19)
- Dermatology (31)
- Dialysis Support Group - “UTSAAH” (11)
- Dietitian (33)
- Emergency Medicine (4)
- Emotional Health (11)
- Endocrinology (33)
- ENT (20)
- Gastroenterology and GI Surgery (53)
- General and Laparoscopic Surgery (21)
- General Surgery (4)
- Gynecology & Obstetrics (183)
- Hematology (20)
- Internal Medicine (294)
- Kidney Transplant (50)
- Kidney Transplantation (20)
- Lung Cancer (8)
- Minimal Invasive Surgery (1)
- Mother & Child (20)
- mucormycosis (5)
- Nephrology (61)
- Neurology (147)
- Neurosurgery (68)
- Nutrition and Dietetics (107)
- Omicron Variant (1)
- Oncology (288)
- Ophthalmology (10)
- Orthopaedics & Joint Replacement (86)
- Paediatrics (59)
- Pediatric Nephrology (3)
- Physiotherapy (5)
- Plastic & Reconstructive Surgery (6)
- Psychiatry and Psychology (90)
- Psychologist (28)
- Pulmonology (72)
- Rheumatology (13)
- Spine Services (21)
- Transradial Angioplasty (16)
- Urology (84)
Query Form
Posted on Apr 19, 2022
Hepatitis due to fats in the body: A Menace often thought little of
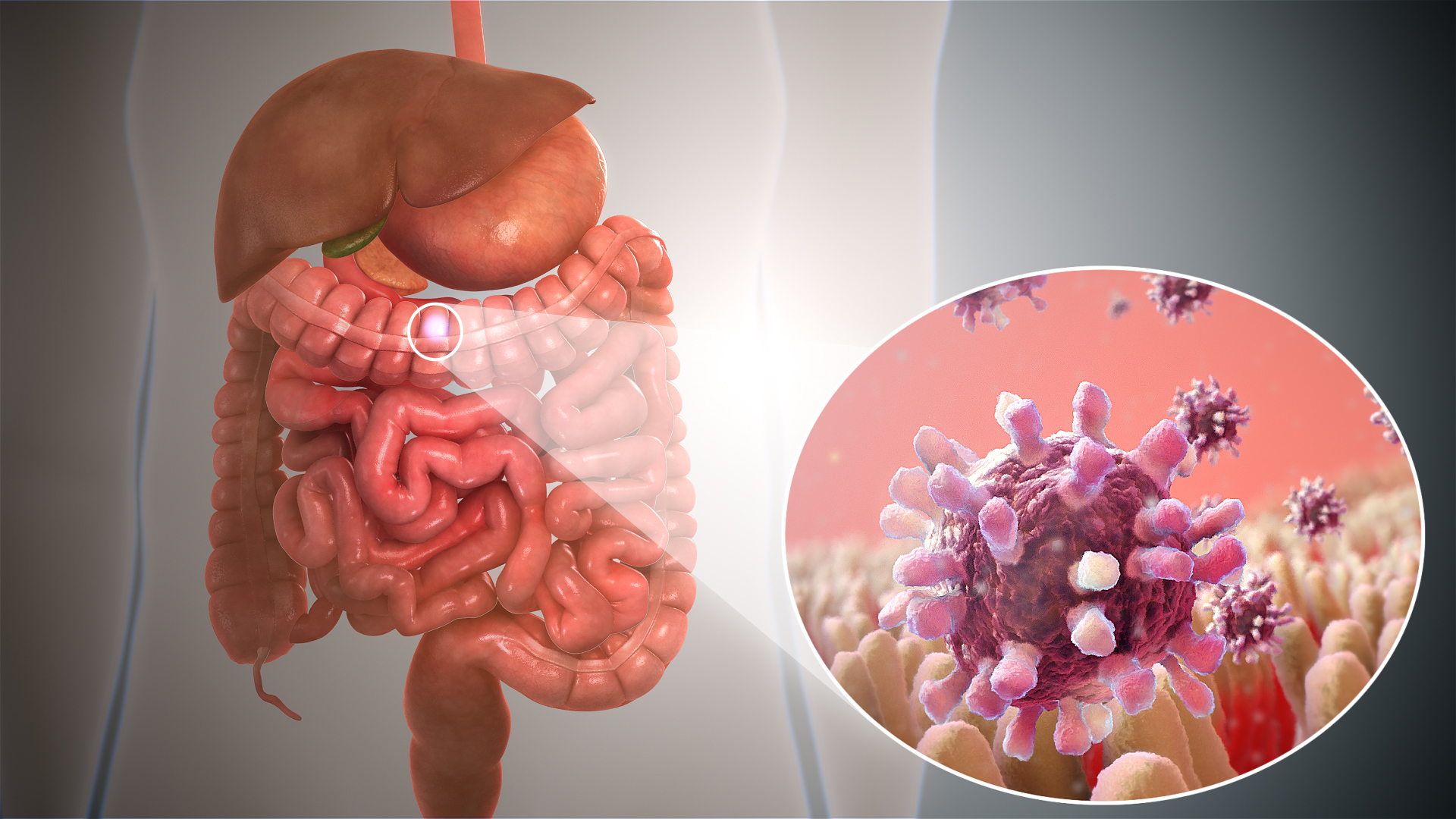
In the ’90s, little was known about the condition called ‘fatty liver’ in a nonalcoholic individual. When I was graduating at a medical college, I used to ignore this topic, and subsequently, used to tell my patients , “Don’t worry, it’s not a problem at all”. Many radiologists actually would not report this condition on ultrasonography thinking it to be a non-significant clinical entity. Today fatty liver disease is believed to the most common cause of chronic liver disease. It constitutes a substantial proportion of patients with what we used to call them cryptogenic cirrhosis. A healthy liver has about 1-3% fat and once it is over 5% it is defined as fatty liver. Nonalcoholic fatty liver disease (NAFLD) represents a spectrum of conditions characterized by fatty liver with or without varying degree of inflammation, liver cell injury and fibrosis. A hepatitis caused by fat is called steatohepatitis. NAFLD is commonly associated with obesity, hyperlipidemia, and diabetes mellitus.

Nonalcoholic Fatty Liver Disease Prevalence:
The prevalence of NAFLD in Indian population ranges from 5% to 28%, which is comparable to the prevalence in West. Furthermore, with a rising incidence of obesity and diabetes in India, the incidence of NAFLD may rise further. Based on data from the National Family Health Survey, the percentage of people who are overweight or obese in India is 12.1% men and 16% women. India is home to around 50 million people with diabetes, which is the largest number in any single country.
Nonalcoholic Fatty Liver Disease & Co morbidity:
What is quite clear now is the fact that NAFLD is no more an innocuous entity and there is a strong association between NAFLD and other potentially life threatening diseases and clinical conditions. Apart from the risk of developing liver cirrhosis and liver cancer, NAFLD is associated with increased risk of death from cardiovascular diseases and extra-hepatic malignancy. It appears that about 9% to 20% of steatohepatitis progresses to cirrhosis in about 15 years. Several studies have documented that the overall mortality in NAFLD patients is higher than the matched healthy control. Overall death from cardiovascular disease in NAFLD ranges from 13% to 30%. NAFLD has been found to be associated with hypothyroidism, polycystic ovary syndrome, gall stone disease and renal dysfunctions. These patients may have health problems directly relating to obesity, which may include arthritis, obstructive sleep apnoea, dyspepsia, gastroesophageal reflux disease, hypetension, adverse pregnancy outcome, dyspnoea on mild exertion, social stigmatization, and depression.
Causes of Nonalcoholic Fatty Liver Disease:
While the cause of NAFLD is still unclear, a diet high in calories, saturated fat and sugar predisposes people for fat accumulation in liver. This is especially true for people who are obese or overweight. There may also be a genetic link that makes some people more susceptible.
Tests to Detect Nonalcoholic Fatty Liver Disease:
Liver ultrasonography, computed tomography scan, magnetic resonance imaging and controlled attenuation parameter using Fibroscan are able to detect fatty liver. Because of ease, ultrasonography is the most commonly used method to diagnose fatty liver. The presence of >33% fat on liver biopsy has been shown to be optimal for detecting fatty liver on ultrasound. While all of these imaging methods can detect a significant accumulation of fat in liver, none can differentiate simple fatty liver from steatohepatitis.
Liver biopsy and histological examination of the liver is the only way to make this distinction. The appropriate treatment of NAFLD is not known. Multiple pharmacologic interventions have been attempted with variable success; these include ursodeoxycholic acid, pentoxiphyllin, vitamin E, and lipid lowering agent. The current management strategies are directed at treating the individual components of the metabolic syndrome. Weight loss through diet control and exercise has been shown to result in improvement of markers of liver inflammation.
Recommendation for Nonalcoholic Fatty Liver Disease:
In conclusion, an incidental detection of fatty liver should not be dismissed as an innocuous condition. Appropriate investigations must be done to assess the severity of liver disease, and also, we should try to look beyond liver considering its strong association with cardiovascular disease and extra-hepatic malignancy.